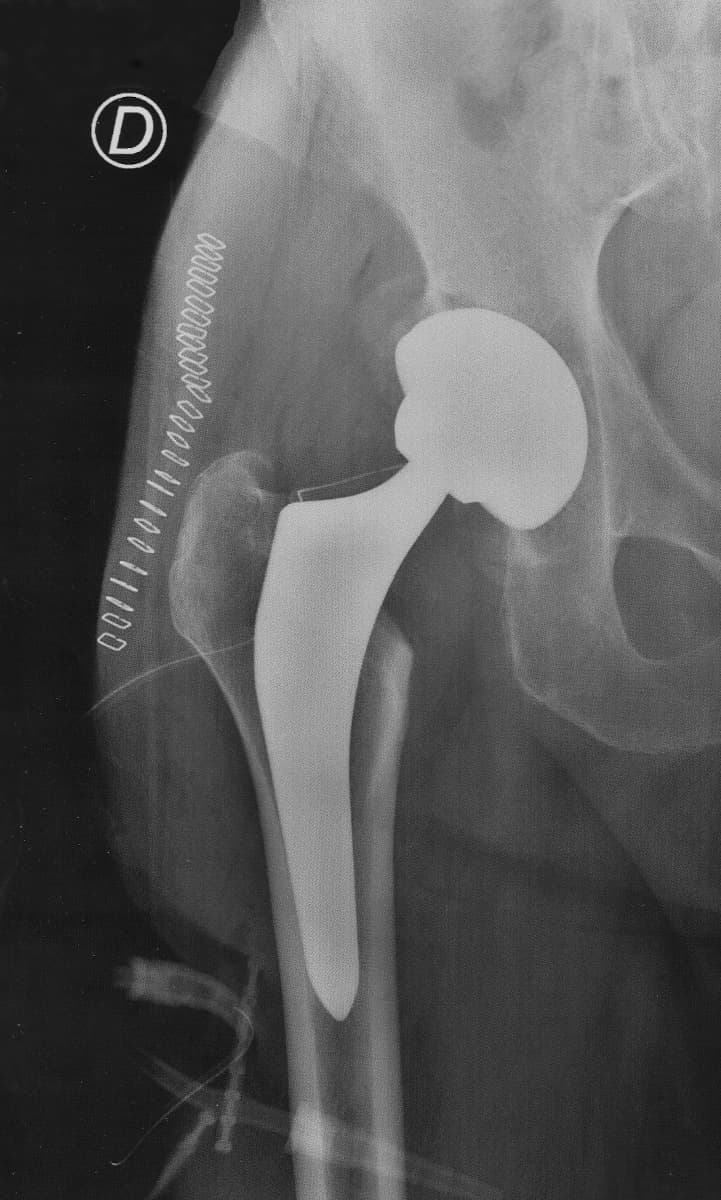
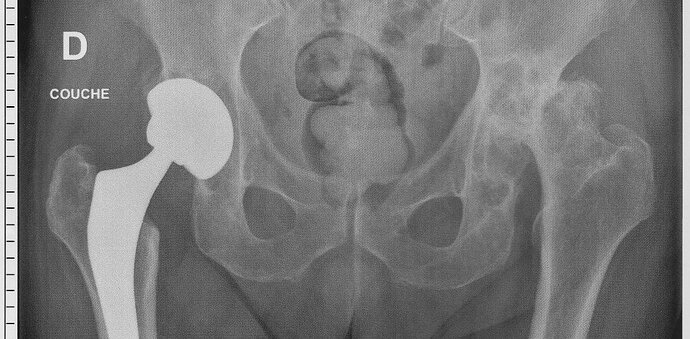
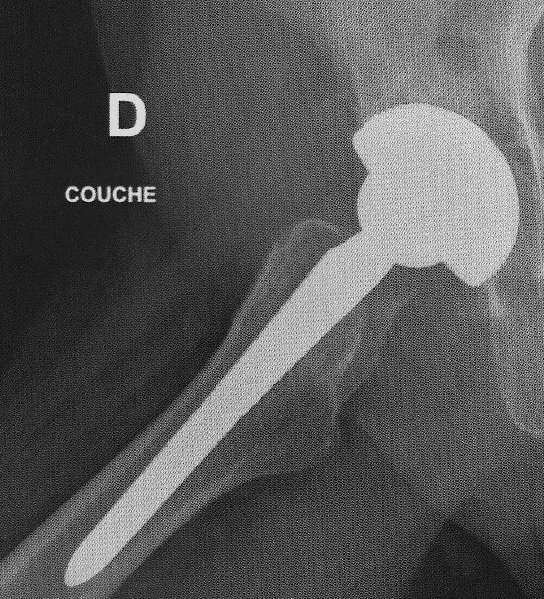
Two weeks ago today, on 2022-11-22, I had a total replacement operation of my right hip. This was more than overdue. Here is a “before” X-ray (click to enlarge) which shows the wreckage of both hip joints.
This image was taken with me lying on my back, with the X-rays projected from top to bottom. Hence, the joint that appears at the left of the image is the right hip joint and vice versa. What is immediately apparent is that the head of the femur (thigh bone), which forms the ball of the ball and socket hip joint (the socket is called the acetabulum of the pelvic bone) is basically gone, leaving the neck of the femur to grind against what was left of the socket. This was extremely painful, and progressed to the point that I could not stand or walk more than about 90 seconds before it became unbearable.
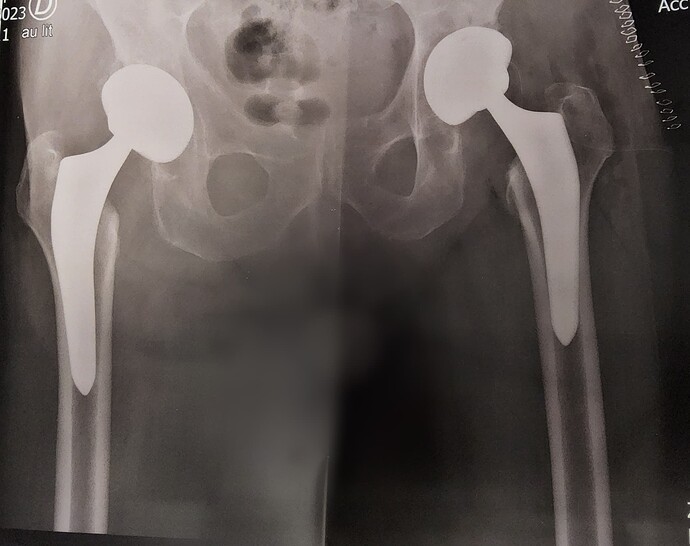
Hip replacement surgery removes the head and neck of the femur and replaces them with an anchor spike that is driven into the core of the long bone, supporting a replacement femur head. These are manufactured from titanium, with surfaces intended to bond to existing bone coated with hydroxyapatite, the mineral that makes up around 70% of natural bone by mass.
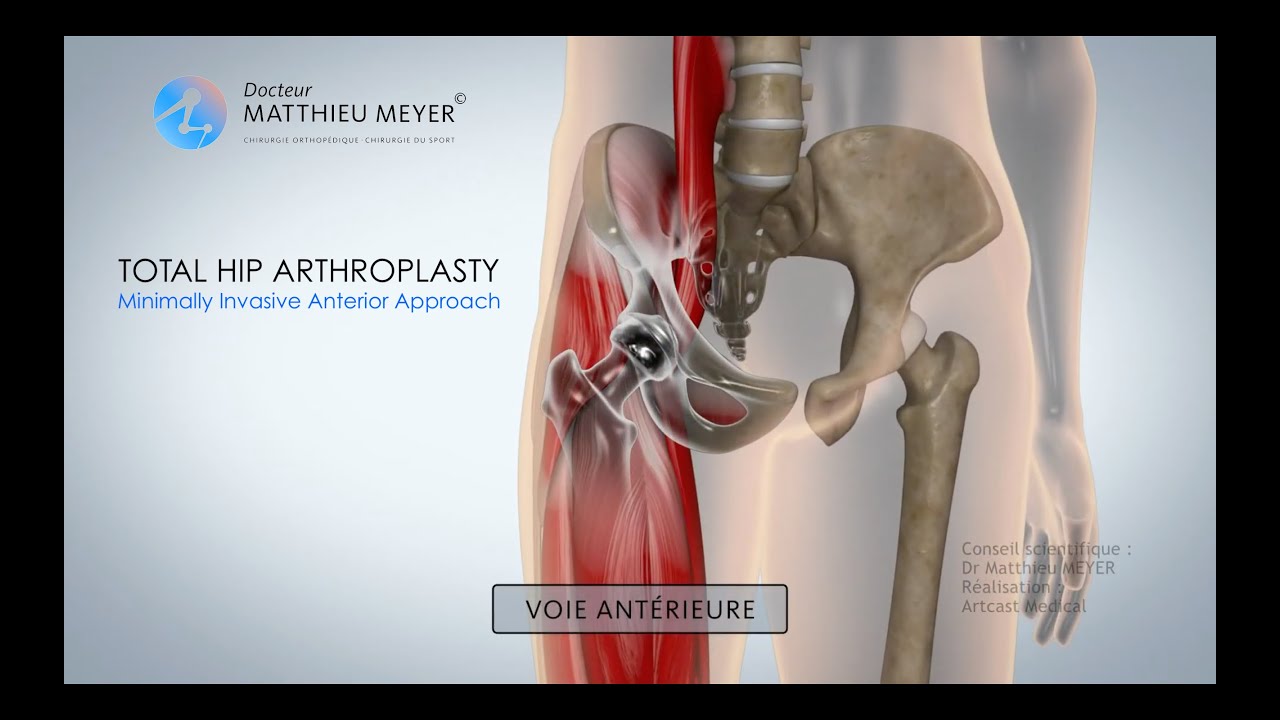
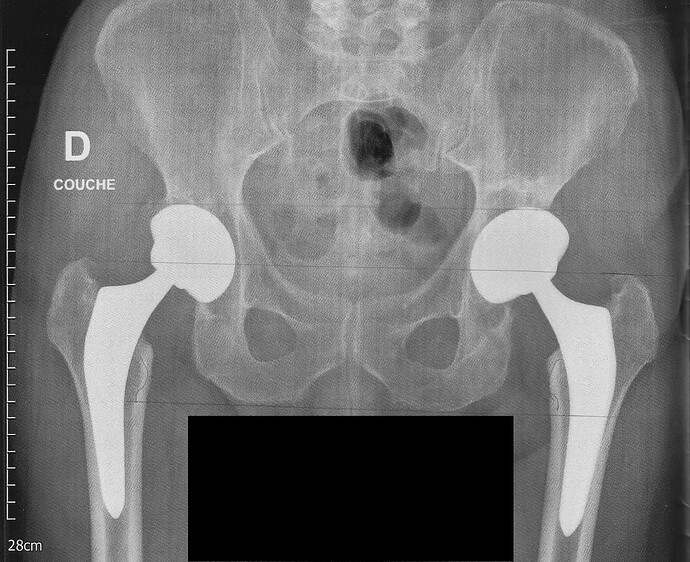
The socket (acetabulum) is reamed out with what amounts to a giant Dremel tool, and a coated titanium replacement socket implanted. A ceramic bearing surface is installed in the socket, which mates to the ball on the replacement femur head. Here is an X-ray of the prosthetic joint after installation.
This is a “non-cemented” prosthesis, which depends upon the natural bone bonding to the hydroxyapatite-coated parts to secure them in place. The orthopedic surgeon believes this produces a stronger and longer-lasting bond than the cemented alternatives or earlier techniques which secured the socket to the pelvis with screws. The rectangular objects at the upper left are the surgical staples used to close the incision; they are scheduled to be removed three weeks after the operation.
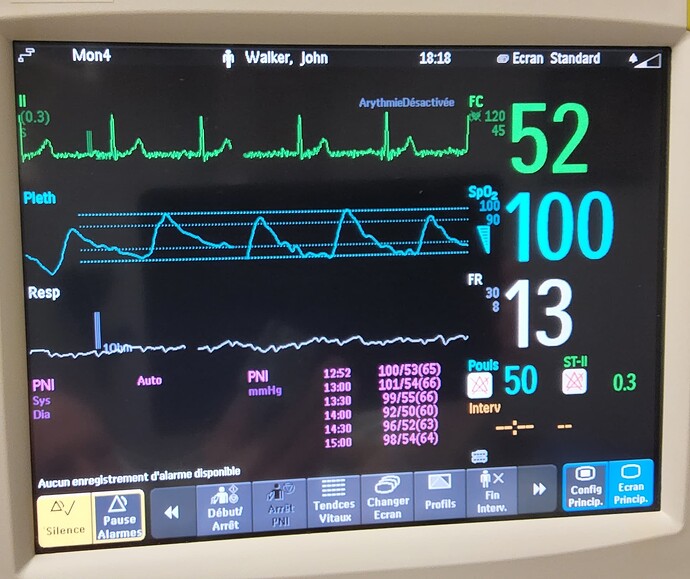
The operation was done using the “minimally invasive anterior approach”. This avoids cutting muscles which usually results in a longer recovery time requiring more physical therapy. The total surgery, which was performed under general anæthesia with propofol (and possibly other agents), took about 90 minutes, and afterward I woke up instantly with no pain. There was no numbness or inability to move my lower extremities, and I was able to walk the next day with the aid of two cane/crutches.
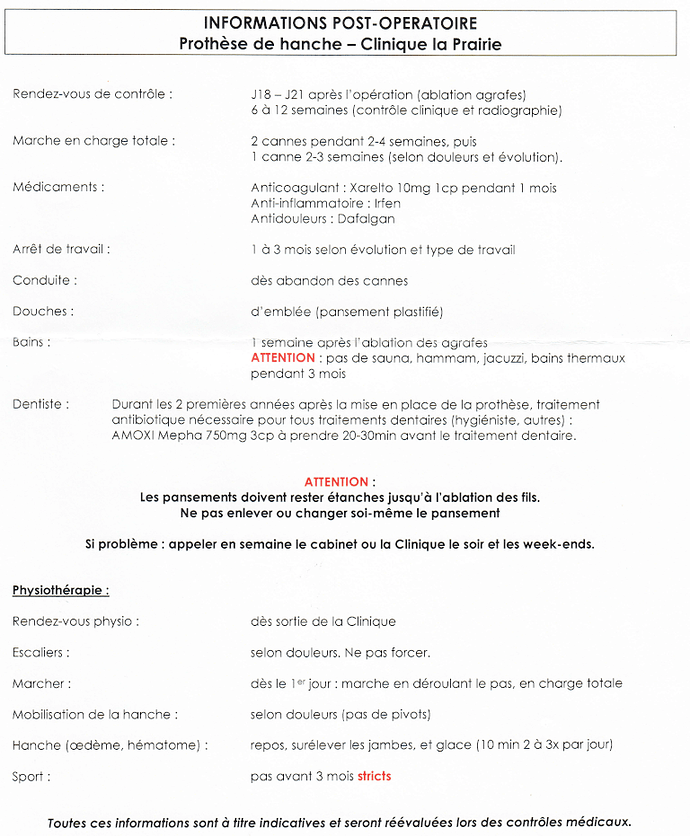
Here is a short video which explains the minimally-invasive anterior approach. The narration is in French, with English subtitles, which I have attempted to enable to show automatically. YouTube subtitle requests are notoriously flaky, so if they don’t appear for you, click the “Gear” link at the bottom right and enable the subtitles manually, or click the “YouTube” link to open a separate player where you can turn them on. I chose this video because it provides the clearest description I’ve seen of the operation in just four minutes.
Here is a video of an actual hip replacement performed using this technique. This is rather gnarly and squeamish viewers should probably give it a pass. The video is “age restricted” by YouTube and cannot be embedded here; click link to view.
Here is the guide (in French) to recuperation after a hip replacement by this technique. The anti-inflammatory “Irfen” is 400 mg ibuprofen, while the analgesic “Dafalgan” is 1g paracetamol. The anti-coagulant “Xarelto” is 10 mg rivaroxaban, taken for 30 days after the operation to reduce the risk of thrombosis. No other pain medication was administered or prescribed after the operation.
Perhaps less apparent from the X-ray at the top, the left hip joint (rightmost in the image) is also a wreck. It started to fail in September 2014, and after an acute phase stabilised as something I’ve been able to live with since then. The plan is that if recovery from the right replacement proceeds as hoped, that one will be replaced in early 2023.